Resources for peri-menopause & menopause. Feel empowered with evidence-based information.
Visit your trusted health professional for a holistic, patient-centred care plan to be the best version of yourself.
menopause 1 0 1
THE THREE STAGES OF MENOPAUSE
PERI MENOPAUSE
-
This is the transition phase leading up to menopause and can last several years.
-
Symptoms such as irregular periods, hot flashes, and mood changes often begin during this stage.
-
Hormonal fluctuations are at their peak here.
MENOPAUSE
-
The moment when 12 consecutive months have passed without a period.
-
Reproductive hormone levels significantly decline.
POST MENOPAUSE
-
The stage after menopause, lasting the rest of your life.
-
Symptoms may ease for some women
-
Reduced hormone levels can lead to long-term health considerations like bone density loss.
AVERAGE AGE AND DURATION
Early Menopause is menopause occurring between 40-45 years.
Premature Ovarian Insufficiency (POI)
is menopause prior to age 40.
Perimenopause is variable and is considered the time leading up to Menopause.
The average age for menopause in most Australians is 51, but it can typically occur anywhere around the late 40s and early 50s.
About Menopause
Early Menopause &
Premature Ovarian Insufficiency
Peri menopause
Diagnosis &
Hormone Testing
Duration
Symptoms
Symptom
ABCs
Menopause is the final menstrual period and usually happens between the ages of 45 and 55 years.
Menopause is typically defined as “The final (last) menstrual period” and is diagnosed 12 months after the final period.
Menopause is a clinical diagnosis, meaning we look at symptoms, menstrual history and determine if you are in-deed menopausal.
-
Measuring hormone levels are generally not indicated because of marked daily fluctuations in their levels.
-
Measuring hormone levels is often unlikely going to change general recommendations & management planning.
-
There can also be a cost for measuring levels & despite paying for the test, it doesn’t always change what we already know & what we would recommend for management.
-
It's important to talk with your health professional about the role of testing and the role it plays in your health care.
Hormone tests typically only ever measured in specific situations in consultation with your doctor, some examples include
-
You are under 40 & we are concerned about pre-mature menopause
-
You no longer have a uterus, so no longer have menstrual bleeds to know if you've hit menopause AND there is marked clinical uncertainty.
-
You are taking progesterone contraception (suppressing the menstrual period) AND there is marked clinical uncertainty.
-
Monitoring certain hormonal treatments.
How long does menopause go for?
-
Menopause is for life. It is diagnosed after 12 months from your last natural menstrual period.
-
There is no reliable way of predicting how long menopausal symptoms will continue for and it varies from person to person.
-
For many, symptoms resolve within 2-5 years.
-
10% to 20% will have symptoms for up to 12 years.
-
The most common prolonged symptoms are vaginal dryness and urinary frequency which may start during the peri-menopause and tend not to resolve naturally with time. There are treatment options for this.
-
For those with symptoms who elect to use treatment, it is advised that you be reviewed annually (yearly) to evaluate your care needs.
-
Preventative health, or prevention of chronic disease, is of most importance in the post-menopausal years.
-
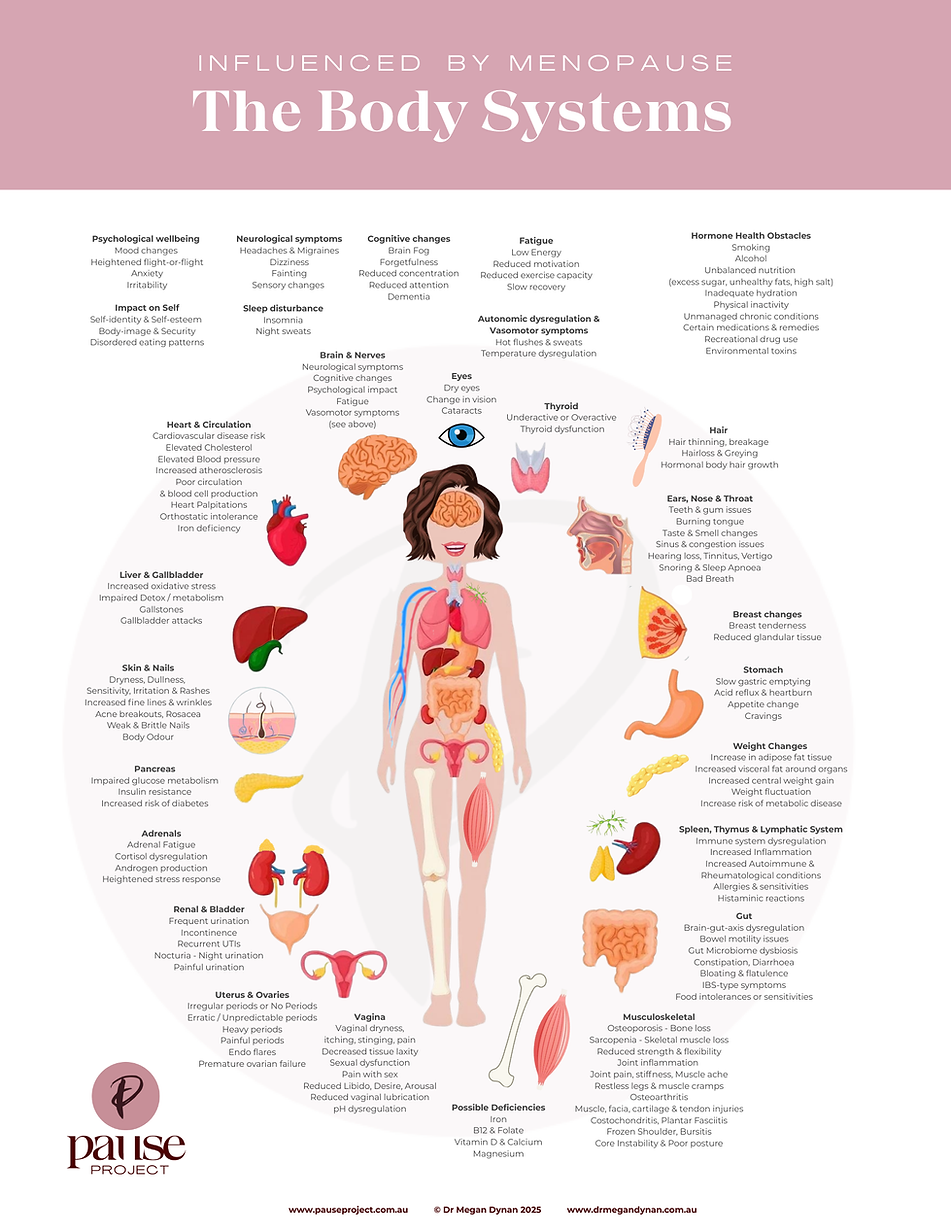
Peri-menopause & menopause can affect multiple body systems impacting on the whole person.
-
Because everyone experiences perimenopause & menopause differently, symptoms experienced can vary from person to person.
-
Some people experience many or all symptoms, and others experience only a few symptoms.
-
We cover symptom management on our website. Navigate to our home page to learn more.
Acne
Hormonal changes can trigger adult acne or other skin concerns during the transition.
Allergies
Some people notice new allergies or worsening of existing ones during menopause.
Anxiety
Heightened worry or nervousness can arise with hormone changes.
Bloating
A feeling of fullness or abdominal swelling, often linked to digestive changes or water retention.
Body Odor
Hormonal fluctuations and increased perspiration can alter personal scent.
Breast Pain / Tenderness
Soreness, throbbing, or tenderness in the breasts may occur, often early in the transition.
Brain Fog / Memory Lapses
Difficulty concentrating, forgetfulness, or feeling mentally “cloudy.”
Brittle Nails
Nails may become weaker, breaking or peeling more easily.
Burning Mouth
A tingling or burning sensation in the mouth or tongue, sometimes accompanied by dry mouth.
Depression
Low mood, sadness, or loss of interest in daily activities can emerge or worsen.
Difficulty Concentrating
Challenges with attention, focus, or clarity of thought.
Digestive Changes
Some people notice indigestion, reflux, nausea, diarrhoea, or constipation.
Dizziness
A sensation of imbalance, light-headedness, or unsteadiness.
Dry or Itchy Eyes
Less tear production can cause dryness, itching, irritation, or light sensitivity.
Dry Skin
Skin may lose elasticity and moisture, leading to dryness or itchiness.
Electric Shock Sensations
Short, sharp tingles under the skin or in muscles, sometimes described as “zaps.”
Fatigue
Ongoing tiredness or low energy, both physical and mental.
Gastrointestinal Problems
Hormone changes can alter digestion and may worsen bloating, gas, or stomach upset.
Hair Loss / Thinning
Hair may become thinner or shed more easily, on the head or body.
Headaches / Migraines
Some people experience worsening headaches or hormone-triggered migraines.
Heart Palpitations
A racing, fluttering, or pounding heartbeat can occur with hormonal shifts.
Hot Flushes
Sudden waves of heat and sweating, often felt in the head, chest, or upper body.
Incontinence / Bladder Changes
Bladder control may weaken, with urgency, leakage, or more frequent infections.
Irregular Periods / Menstrual Changes
Cycles can become heavier, lighter, more frequent, or more spaced out before they eventually stop.
Irritability
Increased frustration, sensitivity, or shorter temper than usual.
Itchy Skin
A tingling, crawling, or itchy sensation on the skin without rash.
Joint Pain / Muscle Aches
Aches, stiffness, or soreness in muscles and joints are common.
Loss of Libido
Reduced interest in sexual activity, often related to hormone changes or vaginal dryness.
Mood Swings
Sudden or extreme shifts in mood or emotions.
Muscle Tension
Tightness, discomfort, or aching in the muscles.
Night Sweats
Hot flushes that occur at night, often disturbing sleep.
Osteoporosis
Declining oestrogen can weaken bones, increasing the risk of fractures.
Panic Attacks
Episodes of intense fear or sudden feelings of panic.
Psychological Changes
Mood changes such as depression, anxiety, irritability, or heightened emotional sensitivity.
Sexual Dysfunction
This can include vaginal dryness, discomfort with sex, or reduced sexual desire.
Sleep Disturbances
Difficulty falling asleep, staying asleep, or waking too early, often linked with night sweats.
Taste Changes
Altered or metallic taste in the mouth, sometimes linked with dry mouth.
Tingling Sensations
“Pins and needles” or shock-like feelings in the hands, feet, arms, or legs.
Urinary Changes
Weaker bladder control, increased frequency, urgency, or susceptibility to infections.
Vaginal Dryness
Less lubrication, thinner tissue, and reduced elasticity can lead to discomfort.
Vasomotor Symptoms
Hot flushes and night sweats together are often grouped as vasomotor symptoms.
Vision Changes
Some people notice blurred vision, light sensitivity, or dry eyes.
Weight Gain / Redistribution
Weight often increases, particularly around the abdomen, due to hormonal and metabolic changes.